Vulvar Cancer
Vulvar cancer is caused by the HPV virus in more than 50% of all cases. 80% of vulvar cancers are in the labia, 10% involve the clitoris and 10% area between the vulva and the anus. The vulva is the skin that surrounds the urethra and vagina on the outer surface of the female genital area.
Types of vulvar cancer include:
Causes of Vulvar Cancer
The cause of vulvar cancer is typically human papillomavirus (HPV) or a genetic mutation in your DNA. DNA mutations cause healthy cells to change and grow at a rapid rate, causing a tumor. Not everyone with HPV will develop vulvar cancer.
Risk Factors for Vulvar Cancer
Some people who get vulvar cancer have a specific mutation in their DNA that increases their risk of getting vulvar cancer. Our hereditary cancer program can provide important information to you and your family so we can identify cancer early, when it is most treatable, and plan your treatment.
Vulvar cancer can be associated with the following risk factors:
- Age.
- HIV infection.
- Many sexual partners.
- Melanoma.
- Sexually transmitted diseases.
- Smoking.

Make an appointment
For more information, please contact your oncologist or the Cancer Care Center aat (859) 301-2237, option 2.
Symptoms of Vulvar Cancer
Most women with early-stage vulvar cancer will have no symptoms. Some women experience itching that will not go away. Symptoms of advanced vulvar cancer include:
- An area on the vulva that looks lighter or darker than the normal.
- A bump or lump that will feel rough or thick.
- An open sore that doesn’t heal.
- Irregular bleeding or discharge.
- Itching.
- Pain or burning.
- Thickening of the vulva.
Diagnosing Vulvar Cancer
If your doctor suspects that you have vulvar cancer, we may run tests to determine the type of cancer and develop the best treatment plan. These tests include:
- Biopsy.
- Blood tests to check genetic makeup and blood markers.
- CT scan.
- MRI.
- PET/CT scan.
- Pelvic exam.
If you’ve been diagnosed with vulvar cancer, we can provide a second opinion and present treatment options.
Treating Vulvar Cancer
At St. Elizabeth Healthcare, we believe in caring for you, not just treating your cancer. Our holistic approach means we combine cancer treatment with working to minimize side effects and help you manage them. Our goal is to make you as comfortable as possible while we use innovative approaches to treat your cancer.
Your treatment plan for vulvar cancer usually begins with surgery. Our surgeons are experts in diagnosing and treating gynecologic cancers.
Depending on the stage of your cancer and whether it has spread, your treatment may include:
Preventing Vulvar Cancer
Steps you can take to reduce your risk of vulvar cancer include:
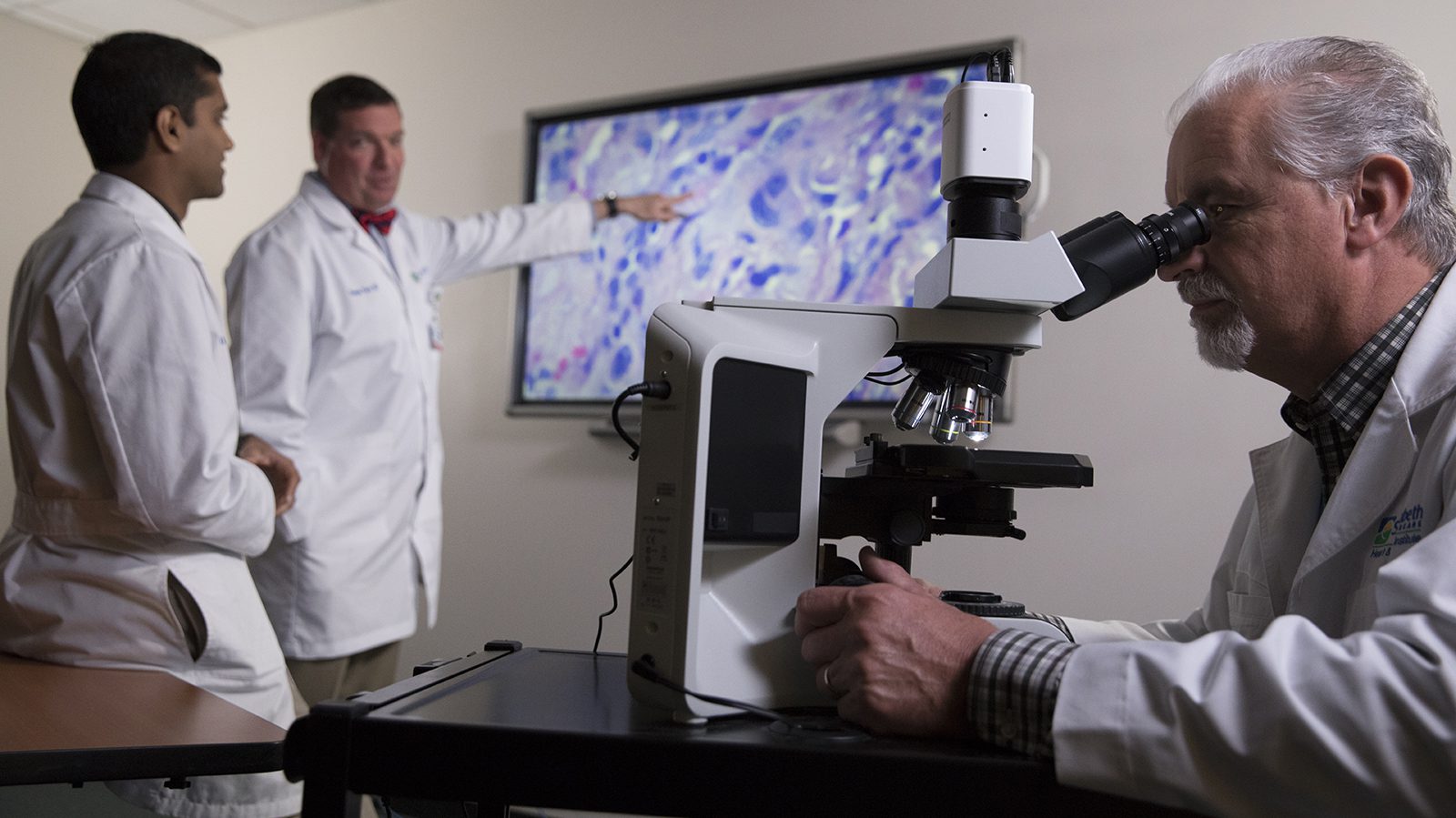
Your Cancer Care Team
The team includes medical oncologists specializing in immunotherapy and precision medicine, surgical oncologists, radiation oncologists, interventional radiologists, thoracic surgeons, pain management specialists, genetic counselors, pathologists, nutritionists, pharmacists, nurses and support staff. They work together to create a treatment plan that’s just right for you.