Ureteral obstruction
Updated: 2024-01-26
Overview
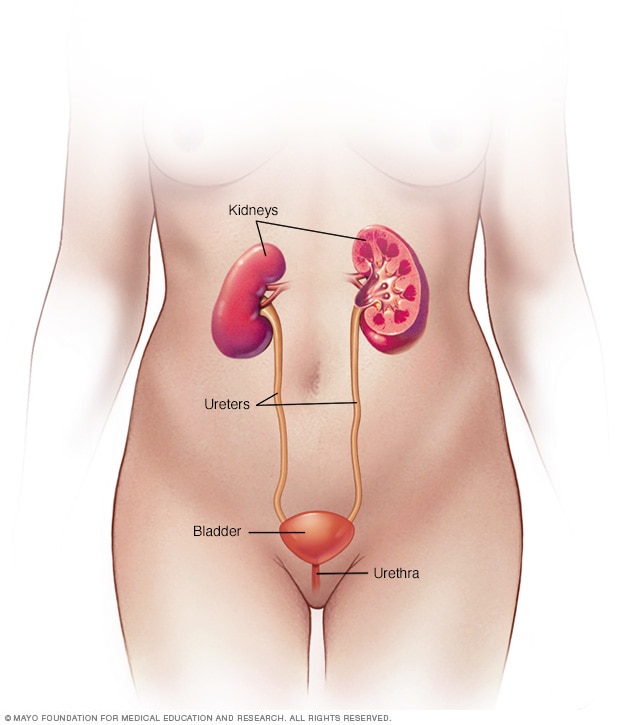
Female urinary system
The urinary system includes the kidneys, ureters, bladder and urethra. The urinary system removes waste from the body through urine. The kidneys are located toward the back of the upper stomach area. They filter waste and fluid from the blood and produce urine. Urine moves from the kidneys through narrow tubes to the bladder. These tubes are called the ureters. The bladder stores urine until it's time to urinate. Urine leaves the body through another small tube called the urethra.
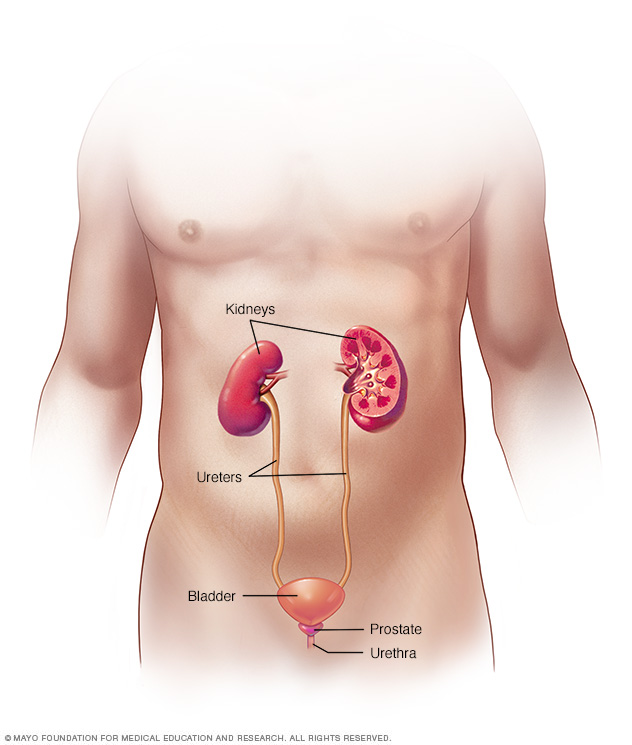
Male urinary system
The urinary system includes the kidneys, ureters, bladder and urethra. The urinary system removes waste from the body through urine. The kidneys are located toward the back of the upper stomach area. They filter waste and fluid from the blood and produce urine. Urine moves from the kidneys through narrow tubes to the bladder. These tubes are called the ureters. The bladder stores urine until it's time to urinate. Urine leaves the body through another small tube called the urethra.
A ureteral obstruction is a blockage in one or both of the tubes (ureters) that carry urine from the kidneys to the bladder. Ureteral obstruction can be cured. However, if it's not treated, symptoms can quickly move from mild — pain, fever and infection — to severe — loss of kidney function, sepsis and death.
Ureteral obstruction is fairly common. Because it's treatable, severe complications are rare.
Symptoms
Ureteral obstruction might have no signs or symptoms. Signs and symptoms depend on where the obstruction occurs, whether it's partial or complete, how quickly it develops, and whether it affects one or both kidneys.
Signs and symptoms might include:
- Pain.
- Changes in how much urine you produce (urine output).
- Difficulty urinating.
- Blood in the urine.
- Urinary tract infections.
- High blood pressure (hypertension).
When to see a doctor
Make an appointment with your health care provider if you have signs and symptoms that worry you.
Seek medical attention if you experience:
- Pain so severe that you can't sit still or find a comfortable position.
- Pain accompanied by nausea and vomiting.
- Pain accompanied by fever and chills.
- Blood in your urine.
- Difficulty passing urine.
Causes
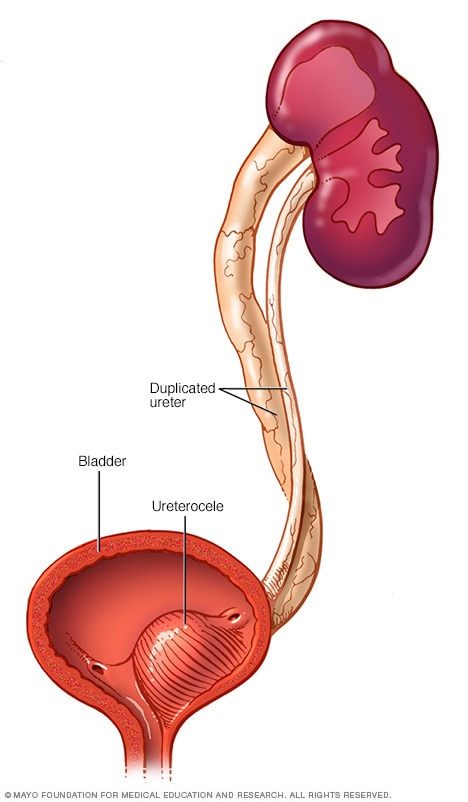
Duplicated ureter and ureterocele
A duplicated ureter occurs when two ureters form on the same kidney. A ureterocele is a small bulge in the ureter, usually in the end closest to the bladder. Both conditions may lead to ureteral obstruction.
Different types of ureteral obstruction have different causes, some of them present at birth (congenital). They include:
- A second (duplicated) ureter. This common condition, which is congenital, causes two ureters to form on the same kidney. The second ureter can be fully or only partially developed. If either ureter doesn't work properly, urine can back up into the kidney and cause damage.
- A blockage (obstruction) where the ureter connects to the kidney or bladder. This prevents urine flow. A blockage where the ureter and kidney meet (ureteropelvic junction) may cause the kidney to swell and eventually stop working. This condition can be congenital or can develop with typical childhood growth, result from an injury or scarring, or in rare cases, develop from a tumor. A blockage where the ureter and bladder meet (ureterovesical junction) may cause urine to back up into the kidneys.
- Ureterocele. If a ureter is too narrow and doesn't allow urine to flow completely, a tiny bulge in the ureter (ureterocele) may develop. When a ureterocele develops, it's usually in the section of the ureter closest to the bladder. This can block urine flow and cause urine to back up into the kidney, possibly leading to kidney damage.
- Retroperitoneal fibrosis. This rare disorder occurs when fibrous tissue grows in the area behind the abdomen. The fibers may grow as the result of cancer tumors or from taking certain medicines used to treat migraines. The fibers encircle and block the ureters, causing urine to back up into the kidneys.
Other possible causes
Various causes inside (intrinsic) or outside (extrinsic) the ureter can lead to ureteral obstruction, including:
- Kidney stones.
- Cancerous and noncancerous tumors.
- Blood clots.
- Enlarged lymph nodes.
- Internal tissue growth, such as endometriosis in females.
- Long-term swelling of the ureter wall, usually due to diseases such as tuberculosis or a parasite infection called schistosomiasis.
Risk factors
Certain conditions present at birth can increase the risk of having ureteral obstruction. Having kidney stones or bladder stones also might increase the risk that one of the ureters becomes blocked. Blood clots, tumors, certain tissue growth and enlarged lymph nodes might also be factors in developing this condition.
Complications
Ureteral obstruction can lead to urinary tract infections and kidney damage, which can be irreversible.
Diagnosis
Often, providers diagnose ureteral obstruction disorders before birth during routine prenatal ultrasounds, which can show details of the developing fetus, including the kidneys, ureters and bladder. Providers often perform another ultrasound after birth to reevaluate the kidneys.
If your provider suspects you have an obstructed ureter, some of these tests and scans might be used to reach a diagnosis:
- Blood and urine tests. Your provider checks samples of your blood and urine for signs of infection and the presence of creatinine, which signals that your kidneys aren't working properly.
- Ultrasound. An ultrasound of the area behind your abdominal organs (retroperitoneal ultrasound) allows your provider to view the kidneys and ureters.
- Bladder catheterization. To test for incomplete or blocked urine flow, your provider inserts a small tube (catheter) through the urethra, injects dye into your bladder, and takes X-rays of your kidneys, ureters, bladder and urethra before and during urination.
- Renal nuclear scan. Your provider or a technician injects a tracer that contains a small amount of radioactive material into your arm. A special camera detects the radioactivity and produces images that your provider uses to evaluate the urinary system.
- Cystoscopy. A small tube with a camera and light is inserted into your urethra or through a small incision. The optical system allows the provider to see inside the urethra and bladder.
- Computerized tomography (CT) scan. A CT scan combines a series of X-ray views taken from many different angles and computer processing to create cross-sectional images of your kidneys, ureter and bladder.
- Magnetic resonance imaging (MRI). An abdominal MRI uses a magnetic field and radio waves to create detailed images of the organs and tissues that make up your urinary system.
Treatment
The goal of ureteral obstruction treatment is to remove blockages, if possible, or bypass the blockage, which may help repair damage to the kidneys. Treatment might include antibiotics to clear associated infections.
Drainage procedures
A ureteral obstruction that causes severe pain might require an immediate procedure to remove urine from your body and temporarily relieve the problems caused by a blockage. Your doctor (urologist) may recommend:
- A ureteral stent, which is a hollow tube inserted inside the ureter to keep it open.
- Percutaneous nephrostomy, during which your doctor inserts a tube through your back to drain the kidney directly (percutaneous nephrostomy).
- A catheter, which is a tube inserted through the urethra to connect the bladder to an external drainage bag. This may be especially important if problems with your bladder also contribute to poor drainage of your kidneys.
Your doctor can tell you which procedure or combination of procedures is best for you. Drainage procedures might provide temporary or permanent relief, depending on your condition.
Surgical procedures
There are a number of surgical procedures used to correct ureteral obstructions. The type of procedure depends on your situation.
Ureteral obstruction surgery may be performed through one of these surgical approaches:
- Endoscopic surgery. This minimally invasive procedure involves passing a lighted scope through the urethra into the bladder and other parts of the urinary tract. The surgeon makes a cut into the damaged or blocked part of the ureter to widen the area and then places a hollow tube (stent) in the ureter to keep it open. This procedure may be done to both diagnose and treat a condition.
- Open surgery. The surgeon makes an incision in your abdomen to remove the blockage and repair your ureter.
- Laparoscopic surgery. In this approach, the surgeon makes one or more small incisions through your skin to insert a small tube with a light, a camera and other instruments needed for the procedure.
- Robot-assisted laparoscopic surgery. The surgeon uses a robotic system to perform a laparoscopic procedure.
The main differences among these surgical approaches are your recovery time after surgery and the number and size of incisions used for the procedure. Your doctor (urologist) determines the type of procedure and the best surgical approach to treat your condition.
Preparing for an appointment
Depending on the frequency and severity of your symptoms, you may make an appointment with your health care provider. Or, you might be referred immediately to a urinary tract specialist (urologist).
Here's information to help you get ready for your appointment.
What you can do
When you make the appointment, ask if there's anything you need to do in advance, such as fasting before having a specific test. Make a list of:
- Your symptoms, including any that seem unrelated to the reason for your appointment.
- Key personal information, including major stresses, recent life changes and family medical history.
- All medications, vitamins or other supplements you take, including the doses.
- Questions to ask your provider.
Take a family member or friend along, if possible, to help you remember the information you're given.
For ureteral obstruction, basic questions to ask your provider include:
- What's likely causing my symptoms?
- Other than the most likely cause, what are other possible causes for my symptoms?
- What tests do I need?
- Is my condition likely temporary or chronic?
- What's the best course of action?
- What are the alternatives to the primary approach you're suggesting?
- I have these other health conditions. How can I best manage them together?
- Are there restrictions I need to follow?
- Should I see a specialist?
- Are there brochures or other printed material I can have? What websites do you recommend?
Don't hesitate to ask other questions.
What to expect from your doctor
Your provider is likely to ask you several questions, such as:
- When did your symptoms begin?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
What you can do in the meantime
Avoid doing anything that seems to worsen your signs and symptoms.