Medulloblastoma
Updated: 2023-01-07
Overview
Medulloblastoma
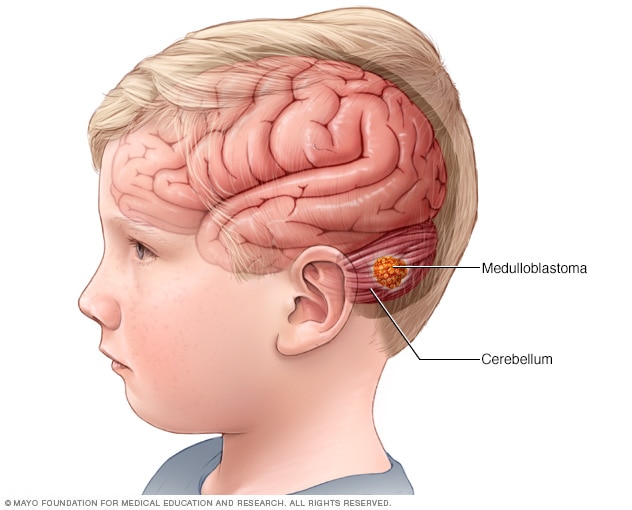
Medulloblastoma is a type of brain cancer that starts in the part of the brain called the cerebellum. Medulloblastoma is the most common type of cancerous brain tumor in children.
Medulloblastoma (muh-dul-o-blas-TOE-muh) is a cancerous brain tumor that starts in the lower back part of the brain. This part of the brain is called the cerebellum. It is involved in muscle coordination, balance and movement.
Medulloblastoma begins as a growth of cells, which is called a tumor. The cells grow quickly and can spread to other parts of the brain. Medulloblastoma cells tend to spread through the fluid that surrounds and protects your brain and spinal cord. This is called cerebrospinal fluid. Medulloblastomas don't usually spread to other parts of the body.
Medulloblastoma can happen at any age, but most often occurs in young children. Though medulloblastoma is rare, it's the most common cancerous brain tumor in children. Medulloblastoma happens more often in families that have a history of conditions that increase the risk of cancer. These syndromes include Gorlin syndrome or Turcot syndrome.
Medulloblastoma symptoms happen when the tumor grows or causes pressure to build up in the brain. They can begin before the cancer is diagnosed and may continue for months or years even after treatment. Signs and symptoms of medulloblastoma may include:
- Dizziness.
- Double vision.
- Headaches.
- Nausea.
- Poor coordination.
- Tiredness.
- Unsteady walk.
- Vomiting.
Diagnosis
The process of diagnosis usually starts with a medical history review and a discussion of signs and symptoms. Tests and procedures used to diagnose medulloblastoma include:
- Neurological exam. During this exam, vision, hearing, balance, coordination and reflexes are tested. This can help show which part of the brain might be affected by the tumor.
- Imaging tests. Imaging tests capture pictures of the brain. The pictures can show the size and location of the tumor. These tests may show pressure or blockages of the cerebrospinal fluid. CTs and MRIs are used for the imaging, but other tests might be needed in certain situations.
- Tissue sample testing. A biopsy is a procedure to remove a sample of the tumor for testing. Biopsies for medulloblastoma are uncommon but might be used in certain situations. In a biopsy, part of the skull is removed. A needle is used to take a sample of the tumor. The sample is tested in a lab to see if it's a medulloblastoma.
- Removal of cerebrospinal fluid for testing. A spinal tap, also called a lumbar puncture, involves inserting a needle between two bones in the lower spine. The needle draws out cerebrospinal fluid from around the spinal cord. The fluid is tested in a lab to look for tumor cells. This test is only done after managing the pressure in the brain or removing the tumor.
Treatment
Treatment for medulloblastoma usually includes surgery followed by radiation or chemotherapy, or both. Your health care team considers many factors when creating a treatment plan. These might include the tumor's location, how fast it's growing, whether it has spread to other parts of the brain and the results of tests on the tumor cells. Your care team also considers your age and your overall health.
Treatment options include:
- Surgery to relieve fluid buildup in the brain. A medulloblastoma may grow to block the flow of cerebrospinal fluid. This can cause a buildup of fluid that puts pressure on the brain. To reduce the pressure, a surgeon can create a pathway for the fluid to flow out of the brain. Sometimes this procedure can be combined with surgery to remove the tumor.
- Surgery to remove the medulloblastoma. The goal of surgery is to remove all of the medulloblastoma. But sometimes it's not possible to fully remove the tumor because it forms near important structures deep within the brain. Most people with medulloblastoma need more treatments after surgery to kill any cancer cells that are left.
- Radiation therapy. Radiation therapy uses powerful energy beams to kill cancer cells. The energy can come from X-rays, protons and other sources. During radiation therapy, a machine directs beams of energy to specific points on the body. Radiation therapy is often used after surgery.
- Chemotherapy. Chemotherapy uses medicines to kill cancer cells. Typically, children and adults with medulloblastoma receive these medicines as an injection into veins. Chemotherapy may be used after surgery or radiation therapy. Sometimes it's done at the same time as radiation therapy.
- Clinical trials. Clinical trials enroll eligible participants to study new treatments or to study new ways of using existing treatments, such as different combinations or timing of radiation therapy and chemotherapy. These studies provide a chance to try the latest treatment options, though the risk of side effects may not be known. Talk with your health care provider for advice.